
Most complications can be avoided by respecting the rectal wall anatomy in the execution of the procedure. Even though SH appears to be promising, we feel that a multicenter randomized study with a long-term follow-up comparing SH and banding is necessary before recommending the procedure. The most common complication in the first 25 cases of the surgeon's experience was bleeding (48%). Most complications (65%) occurred after the surgeon had more than 25 case experiences of stapled hemorrhoidectomy. Fissure was treated by dilatation in 57%. Anal stenoses were treated by dilatation in 55% and by anoplasty in 45%. As complication, bleeding was determined in 13 (20) patients, pain was in 6 (9), urinary. Few complications were specific to stapled hemorrhoidopexy however, these included failure of the stapling gun, urosepsis, and pelvic sepsis. All hemorrhoidal thromboses were excised. One or more complication developed in total 17 (26) patients.

Recurrent hemorrhoids were treated by ligation in 40% and by Milligan-Morgan procedure in 32%. The most common complication after 1 week was recurrence of hemorrhoids in 2.3% of patients, severe pain (1.7%), stenosis (0.8%), fissure (0.6%), bleeding (0.5%), skin tag (0.5%), thrombosis (0.4%), papillary hypertrophy (0.3%) fecal urency (0.2%), staples problems (0.2%), gas flatus and fecal incontinence (0.2%), intramural abscess, partial dehiscence, mucosal septum and intussusception (each <0.1%). One patient with anastomotic dehiscence needed pelvic drainage and colostomy formation. Bleeding was treated surgically in 24%, with Foley insertion 15% and by epinephrine infiltration in 2% 53% of patients with bleeding received no treatment and 6% needed transfusion. Immediate complications (first week) were: severe pain in 5.0% of all patients, bleeding (4.2%), thrombosis (2.3%), urinary retention (1.5%), anastomotic dehiscence (0.5%), fissure (0.2%), perineal intramural hematoma (0.1%), and submucosal abscess (0.1%). A review of 1,107 patients treated with SH from twelve Italian coloproctological centers has revealed a 15% (164/1,107) complication rate. The unusual complications described (rectal perforation, pelvic sepsis, rectovaginal fistulas) might suggest that the operation should be performed by experienced colorectal surgeons who are familiar with the technique and aware of the possible complications.Stapled hemorrhoidectomy (SH), a new approach to the treatment of hemorrhoids, removes a circumferential strip of mucosa about four centimeters above the dentate line. The complications are similar to those of other techniques and are easily resolved. Stapled hemorrhoidopexy is a significantly less painful operation and offers significant advantages in terms of hospital stay and symptom control in the long term, making for a significantly earlier return to work. In 3 cases we underestimated the extent of the mucosal prolapse and the patients were reoperated on by stapled transanal rectal resection after one (2 patients) and two years. We had one case of rectovaginal fistula in a young woman. The risks of stapled hemorrhoidectomy include bleeding, infection, anal fissuring (tearing of the lining of the anal canal), narrowing of the anal or rectal. Complete or incomplete recurrence occurred in 10 cases (2.2%). Severe pain, when present, may depend on technical failure or learning curve.
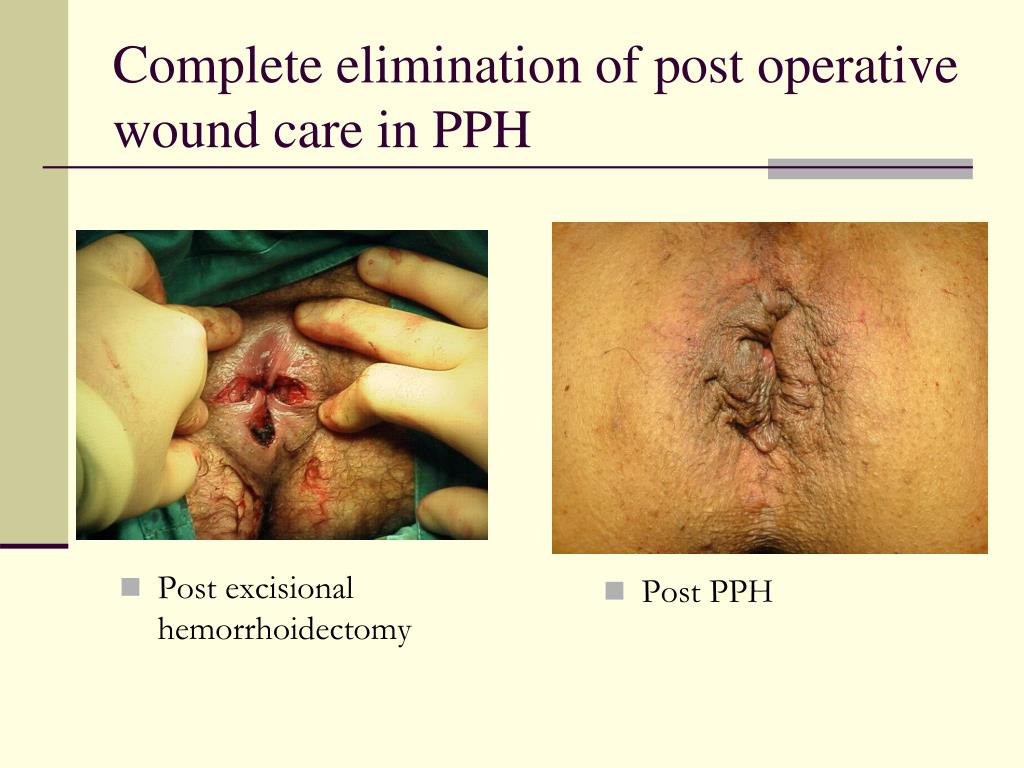
Urge to defecate, although present in 14% of patients, disappears in a few weeks. Bleeding in the early postoperative period occurred in 3.9% of all patients and in 7 cases (1.5%) reoperation was necessary. Patient's satisfaction is the best response to all criticism. A visual analog scale was used for postoperative pain scoring. Patients were assessed by structural interview to assess their symptoms before and after surgery, and surgical and functional outcome was assessed at 1, 3, 6, 12 and 24 months. Four hundred and forty-nine patients with haemorrhoids of all degrees and mucosal rectal prolapse were treated at our institution over a five-year period (1999-2004). The follow-up shows better symptom control than other surgical techniques. Stapled hemorrhoidopexy (SH) presents a number of complications which differ from those of traditional haemorrhoidectomy (Milligan-Morgan, diathermy haemorrhoidectomy).


 0 kommentar(er)
0 kommentar(er)
